News
Newswise — Bethesda, Md. —
Researchers from Oregon Health and Science University and Oregon State University have found that aspirin may slow the spread of some types of colon and pancreatic cancer cells. The paper is published in the American Journal of Physiology—Cell Physiology.
Platelets are blood cells involved with clotting. They promote the growth of cancerous cells by releasing growth factors and increasing the response of certain proteins that regulate tumor cell development (oncoproteins). Low doses of aspirin, an anti-platelet drug, have been shown to reduce the risk of some types of gastrointestinal cancers, but the process by which aspirin hampers tumor growth has been unclear. “The current study was designed to determine the effect of inhibition of platelet activation and function by aspirin therapy on colon and pancreatic cancer cell proliferation,” the researchers wrote.The research team combined activated platelets primed for the clotting process with three groups of cancer cells:• metastatic colon cancer (cells that have spread outside the colon),• nonmetastatic colon cancer (cells that grow only within the colon) and• nonmetastatic pancreatic cancer cells.
When they added aspirin to the mixture, they found that the platelets were no longer able to stimulate growth and replication in the pancreatic and nonmetastatic colon cancer cells. The metastatic colon cancer cells continued to multiply when treated with aspirin.
In pancreatic cancer cells, low doses of aspirin stopped the platelets from releasing growth factor and hampered the signaling of the oncoproteins that cause cancer to survive and spread. Only very high doses—larger than are possible to take orally—were effective in stopping growth in the metastatic colon cells, explained the researchers.
The findings detail the interaction among platelets, aspirin and tumor cells and are promising for the future treatment of nonmetastatic cancer, according to the researchers. “Our study reveals important differences and specificities in the mechanism of action of high- and low-dose aspirin in metastatic and nonmetastatic cancer cells with different tumor origins and suggests that the ability of aspirin to prevent platelet-induced c-MYC [an oncoprotein] expression might be selective for a nonmetastatic phenotype.”
Read the full article, “Aspirin therapy reduces the ability of platelets to promote colon and pancreatic cancer cell proliferation: implications for the oncoprotein c-MYC,” published ahead of print in the American Journal of Physiology—Cell Physiology.
Newswise — Philadelphia, –
Nationally, the highest rates of asthma-related deaths and hospitalizations are among low-income minority adults, but most existing research doesn’t focus on these patients. In particular, studies may not investigate patients where they live, in complicated, difficult circumstances. Many adult asthma patients have multiple diseases and exposure to tobacco smoke, but much research reflects the convenience of recruiting patients in clinics and on the relative simplicity of studying patients who do not have accompanying diseases such as hypertension, diabetes, and obesity.
A new study analyzes patients at ground level, drawing on reports from community health workers who visit asthma patients at home, where extreme living conditions such as poor housing, neighborhood violence, and lack of social support impose steep barriers to public health care, as well as to high-quality research. The research team argues that home visits offer a fuller understanding of how the social environment of asthma patients impacts their overall health.
Researchers from the Community Asthma Prevention Program (CAPP) at Children’s Hospital of Philadelphia (CHOP) and the Perelman School of Medicine at the University of Pennsylvania describe those challenges in a study in the December 2016 issue of the Journal of Allergy and Clinical Immunology. The authors focused on 301 adults living in low-income Philadelphia neighborhoods who were prescribed an inhaled corticosteroid for asthma and required oral steroids for an exacerbation and/or had an emergency or inpatient visit within the last six months.
Community health workers visited patients in their homes and found 71 percent rented, with many living in one-room apartments or overcrowded spaces with multiple family members. Many patients also live in typical Philadelphia rowhomes, which were built in the late 19th century and are difficult to maintain on a limited income. These patients are routinely exposed to common indoor asthma triggers, such as rodents, roaches, and mold. Only 25 percent of people who participated in the study were currently employed either part or full-time. Community health workers reported their impressions of these stark, and sometimes bleak, living conditions:
“It’s not just the finances, it’s the violence, lack of education and job opportunities.”“Homes are in poor repair. Some are just unlivable.”“Depression survey seems to trigger a lot of emotions. Often patients are crying as we try to complete it.”
“Many of these patients start to feel a sense of hopelessness, especially the very sick,” says Tyra Bryant-Stephens, MD, corresponding author and medical director of CAPP at CHOP. “They feel there is very little possibility of changing their current living situation, which includes poor housing, exposure to violent crime, and limited access to transportation. Some of these living conditions make it difficult or impossible for patients to get to their medical visits, which results in a further decline of their health.”
Living in a high-stress environment encourages many patients to continue smoking, despite knowing it contributes to their asthma symptoms. Twenty-eight percent of those surveyed admitted they currently smoke. Other issues community health workers encountered were low education rates, limited access to healthy foods, and poor general health; 58 percent of patients had hypertension and 32 percent had diabetes.
“Medical personnel no longer make house calls, so this research gives us a view of how poverty, unfavorable home conditions, and lack of social resources limit patients’ ability to access healthcare,” says Andrea J. Apter, MD, MSc, MA, principal investigator of the study and Chief of the Section of Allergy & Immunology at the Perelman School of Medicine at the University of Pennsylvania. “Without the knowledge of these barriers, health providers do not have the information needed to create a tailored and empathetic approach to asthma management.”
Bryant-Stephens adds, “As long as there is poor housing, health disparities will continue to exist, despite medical advancements being made in the fight against asthma. The issue is not limited to Philadelphia and needs to be addressed on a national scale. Without addressing poor housing, we will never be able to truly eliminate disparities in outcomes among adult asthma patients.”
Research reported was funded through a Patient-Centered Outcomes Research Institute (PCORI) Program Award.
Tyra Bryant-Stephens, Shakira Reed-Wells, Maryori Canales, Luzmercy Perez, A. Russell Localio, Andrea J. Apter. “Home Visits are Needed to Address Asthma Health Disparities in Adults,” Journal of Allergy and Clinical Immunology. Published December 2016. http://dx.doi.org/10.1016/j.jaci.2016.10.006
# # #
Newswise — Rockville, Md. —
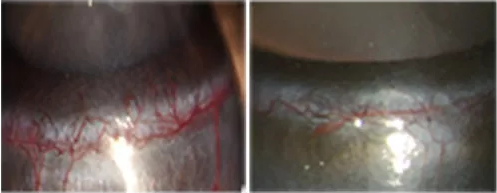
Vision scientists may have discovered how to reduce pedestrian collisions in crowded and chaotic open space environments like bus terminals, shopping malls and city plazas involving individuals with partial blindness. Researchers have determined from which direction collisions with partially blind pedestrians are most likely to originate. This understanding will guide the development of new glasses that expand the sight of a person with limited peripheral vision.
The paper, titled “The risk of pedestrian collisions with peripheral visual field loss” was recently published in the Journal of Vision. The authors created a mathematical model to determine collision risk and compared that risk to the limited vision of 42 patients with retinitis pigmentosa.
“We found that the risk of collision is highest from pedestrians at an angle of 45 degrees from the patient’s walking path,” says lead author Eli Peli, OD, professor of ophthalmology at the Schepens Eye Research Institute, Massachusetts Eye and Ear, Harvard Medical School. “This means that any visual-field expanding device will be most effective if it can cover that angle.”
Peli and his colleagues are developing new devices based on prism-containing eyewear they previously designed. Prisms are primarily prescribed to correct visual defects by bending light. To minimize the loss of peripheral vision, new prism-containing glasses would bend light to hit areas of the eye that still function, expanding what a patient could see.
Patients with blindness in the left or right half of one of their eyes (hemianopia) caused by a stroke, brain tumor or trauma, or patients with limited peripheral vision from retinitis pigmentosa, Usher syndrome, choroideremia and advanced glaucoma may one day benefit from the vision-expanding devices currently under development.
###
Newswise —
Bai jiu (白酒) are distilled spirits made and used throughout rural China for everyday use and special occasions. Distillation of bai jiu is regulated lightly or not at all and nearly every town or village has a distiller. Little is known about the composition of these Chinese spirits, a gap this study seeks to fill given the health risks associated with their high ethanol and high acetaldehyde concentrations.
Researchers purchased 61 samples of Chinese white spirits from small-factory scale producers in central China, and an independent laboratory conducted analyses. Alcohol strength was determined by hydrometer. Gas chromatography was used to determine the concentration of volatile organic compounds: ethanol, methanol, acetaldehyde, ethyl acetate, and higher alcohols. Atomic absorption spectroscopy was used to determine the concentration of lead, arsenic, and cadmium. Guidelines developed by the Alcohol Measures for Public Health Research Alliance (AMPHORA) of the European Commission were used to assess risk.
Results showed that alcohol strength ranged from 35.7 to 61.4 percent, and 58 of the 61 samples exceeded 40 percent. Although the concentration of methanol, ethyl acetate, lead, arsenic, and cadmium were below AMPHORA limits, 40 of the 61 samples had acetaldehyde levels above these limits. The high ethanol concentrations, coupled with a high percentage of samples with elevated acetaldehyde levels, have cumulative long-term health risks, particularly for the substantial proportion of people in China with a genetic trait for impaired acetaldehyde metabolism.
SEE ORIGINAL STUDY
Newswise — Boston, Mass. —
Massachusetts Eye and Ear recently opened the Center for Thyroid Eye Disease and Orbital Surgery, a multidisciplinary initiative to address complex conditions affecting the eye sockets, including orbital tumors and thyroid eye disease. Led by world-renowned experts with specialized training in ophthalmic plastic surgery, endoscopic orbital surgery, strabismus, thyroid gland disorders, neurosurgery and head and neck oncology, the Center will not only provide high quality care to patients with these conditions in one location, but will also support and promote an environment for pioneering novel treatments to improve upon current treatment strategies. The Center is based at the main campus of Mass. Eye and Ear at 243 Charles Street.
“Thyroid eye disease and tumors of the eye socket (orbit) are complicated, and potentially sight threatening, clinical conditions,” said Suzanne Freitag, M.D., Director of the Ophthalmic Plastic Surgery Service and Co-director of the Center for Thyroid Eye Disease and Orbital Surgery at Mass. Eye and Ear and Associate Professor of Ophthalmology at Harvard Medical School (HMS). “The Center is one of the largest and most comprehensive of its kind in the United States that offers convenient, closely coordinated, subspecialty care and treatments that patients can readily access from a single location.”
Thyroid eye disease is an inflammatory condition involving both the thyroid gland and the eye sockets. Patients often experience severe inflammation of the eye sockets and surrounding tissues that can cause a multitude of problems including disabling double vision or permanent vision loss. Advanced medical and surgical therapies may be necessary to manage this disease and preserve visual function.
Orbital tumors can affect the bones of the eye socket, the eyeball, the eye socket muscles, the optic nerve and the surrounding fat and can cause a number of symptoms, including double vision or bulging eye. Surgeons at Mass. Eye and Ear are pioneering minimally invasive surgical techniques to remove these tumors and speed up recovery time. They are also well equipped to provide care to patients with vascular and lymphatic orbital malformations, a rare subset of orbital tumors that require highly specialized care.
“Our team of multidisciplinary experts is conducting evidence-based research and pioneering minimally invasive, surgical techniques that are rapidly changing how we deliver care to our patients,” said Benjamin Bleier, M.D., an Assistant Professor of Otolaryngology at HMS and a nationally renowned endoscopic sinus and skull base surgeon. “These innovations are resulting in less pain, a faster recovery time, and overall better quality of care for our patients.”
Dr. Bleier co-directs the Center with Dr. Freitag and Dean Cestari, M.D. Dr. Cestari is an Assistant Professor of Ophthalmology at HMS, and one of a handful of clinicians in the country who is board certified in both neurology and ophthalmology.
“We are very fortunate to have physicians who are constantly pushing the envelope in the way we approach complex patient care through research and collaboration,” said John Fernandez, President and CEO of Mass. Eye and Ear. “The Center for Thyroid Eye Disease and Orbital Surgery represents a marriage of ophthalmology and otolaryngology care that will ensure that we’re delivering the highest quality of care for Mass. Eye and Ear patients."
To Make an Appointment:617-573-5529
About Massachusetts Eye and EarMass. Eye and Ear clinicians and scientists are driven by a mission to find cures for blindness, deafness and diseases of the head and neck. Now united with Schepens Eye Research Institute, Mass. Eye and Ear is the world's largest vision and hearing research center, developing new treatments and cures through discovery and innovation. Mass. Eye and Ear is a Harvard Medical School teaching hospital and trains future medical leaders in ophthalmology and otolaryngology, through residency as well as clinical and research fellowships. Internationally acclaimed since its founding in 1824, Mass. Eye and Ear employs full-time, board-certified physicians who offer high-quality and affordable specialty care that ranges from the routine to the very complex. In the 2016–2017 “Best Hospitals Survey,” U.S. News & World Report ranked Mass. Eye and Ear #1 in the nation for ear, nose and throat care and #1 in the Northeast for eye care. For more information about life-changing care and research, or to learn how you can help, please visit MassEyeAndEar.org.
Newswise — CHAPEL HILL, NC –
A majority of adolescents in the United States report current cigar warning labels to be very believable, according to a new study conducted by doctors and researchers at the University of North Carolina-Chapel Hill. But significant differences exist in the believability of specific cigar warnings, suggesting that more work is needed to establish the best warnings to dissuade youth from smoking cigars.
The study, published in the Journal of Adolescent Health, included a national phone survey of 1,125 adolescents from ages 13 to 17. The survey presented individuals with one of three current cigar health warnings that specifically isolate the risk of cigar smoke:
• Cigar smoking can cause cancers of the mouth and throat, even if you do not inhale• Cigar smoking can cause lung cancer and heart disease. • Cigars are not a safe alternative to cigarettes.
The surveyors then asked a number of questions about the believability of the warnings. Three quarters (76.7 percent) of all respondents found it very believable that “cigar smoking can cause lung cancer and heart disease,” while just 53.4 percent found it very believable that “cigar smoking can cause cancers of the mouth and throat, even if you do not inhale” and only 49.8 percent found it very believable that “cigars are not a safe alternative to cigarettes.”
Respondents were classified as either susceptible – meaning they had used a cigarette or expressed interest in trying one – or non-susceptible. About 17 percent of those surveyed were classified as “susceptible.” Adolescents susceptible to using cigarettes were significantly less likely to report the cigar warnings to be very believable. The potential source of the cigar warning (FDA, CDC, the Surgeon General, or none) did not impact surveyors’ answers, nor did their race, age, or sex.
Studies have shown that cigars are one of the most common tobacco products among adolescents in the U.S., with one in 12 adolescents reporting current use of a cigar product.
“This is the first research that has been done to track how young people perceive cigars warning labels,” said Sarah Kowitt, doctoral candidate at the UNC Gillings School of Global Public Health and lead author of the study.
“Adolescents may be misguided about the safety of cigar use,” said Adam O. Goldstein, MD, MPH, study co-author, professor of family medicine, and member of the UNC Lineberger Comprehensive Cancer Center. “Many still believe that risks of cigars can be mitigated by not inhaling or inhaling less. But we know that cigar smoking can cause serious harm, including cancer and heart disease.”
Historically, most tobacco prevention campaigns have been aimed at cigarettes. Some states, such as Maryland, have rolled out cigar-specific campaigns that may help dismantle cigar myths among youth.
While the current cigar warnings were mostly seen as believable, Goldstein said that further study is needed, especially on the impact of graphic cigar warnings in addition to text. Also, the UNC researchers suggest continued study to develop warnings that have the maximum impact on susceptible adolescents.
Some countries, such as Australia, have begun this work. “In Australia, warnings include pictorial representations, which may engage adolescents more effectively,” Goldstein said.
Other UNC researchers on the study include Kristen Jarman, MSPH, and Leah Ranney PhD.This research was supported by grant number P50CA180907 from the National Cancer Institute and FDA Center for Tobacco Products (CTP).
Newswise —
Alcohol is the most commonly used psychoactive substance among older adults, and this group can have unique risks associated with alcohol consumption—in even lower amounts—compared to younger persons.
“Older adults have particular vulnerabilities to alcohol due to physiological changes during aging, including increasing chronic disease burden and medication use,” said Benjamin Han, MD, MPH, a geriatrician and health services researcher at the Center for Drug Use and HIV Research (CDUHR) and in the Division of Geriatric Medicine and Palliative Care at NYU Langone Medical Center (NYU Langone). “However, no recent studies have estimated trends in alcohol use, including binge alcohol use and alcohol use disorders among older adults.”
To address the lack of research, Dr. Han and his team examined data from the National Survey on Drug Use and Health (years 2005 to 2014) in a paper published in the journal Drug and Alcohol Dependence. Trends of self-reported past-month binge alcohol use and alcohol use disorder were examined among adults age 50 and older. The researchers found significant increases in past-year alcohol use, past-month alcohol use, past-month binge drinking, and alcohol use disorders. The paper, “Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014.” Published on-line 12 December 2016.
Results also suggest that while men had a higher prevalence of binge alcohol use and alcohol use disorders than women, binge alcohol use and alcohol use disorder increased among women in this nationally representative sample.
“As females age, they tend to experience a larger impact of physiological changes in lean body mass compared to men,” commented Dr. Han. “Thus, they may experience the adverse effects associated with consuming alcohol even in lower amounts.”
“The increase in binge drinking among older women is particularly alarming” said Dr. Palamar, PhD, MPH, a CDUHR affiliated researcher and an assistant professor of Population Health at NYU Langone. “Both men and women are at risk for getting themselves into risky sexual situations while drinking, but women are at particularly high risk.” Dr. Palamar also stated that “heavy drinking can not only have unintended health consequences, but it can also lead to socially embarrassing or regretful behavior.”
For the researchers, the results also raise public health concerns, given the significant increases in binge alcohol use among older adults who reported “fair/poor” health and/or multiple chronic conditions. This population is particularly vulnerable to the negative effects of alcohol as it can impact chronic disease management or increase the risk of injury.
“Health care providers need to be made aware of this increasing trend of unhealthy alcohol use, particularly among older females, and ensure that screening for unhealthy alcohol use is part of regular medical care for this population” said Dr. Han.
Researcher Affiliations: Benjamin H. Han1,2, Alison A. Moore3, Scott Sherman1,4, Katherine M. Keyes5, Joseph J. Palamar2,4
1. New York University School of Medicine, Department of Medicine, Division of Geriatric Medicine and Palliative Care, 550 First Avenue, BCD 615, New York, NY 100162. Center for Drug Use and HIV Research, New York University Rory College of Nursing, 433 First Avenue, 7th Floor, New York, NY 10010.3. University of California, San Diego, Department of Medicine, Division of Geriatrics, 9500Gilman Drive, La Jolla, CA 920934. New York University Langone Medical Center, Department of Population Health, 550 First Avenue, New York, NY 100165. Columbia University, Mailman School of Public Health, 722 West 168th Street, New York, NY 10032
This project was funded, in part, by the NIH (K01 DA-038800, PI: Palamar).
About NYU Langone Medical Center: NYU Langone Medical Center, a world-class, patient-centered, integrated academic medical center, is one of the nation’s premier centers for excellence in clinical care, biomedical research, and medical education. Located in the heart of Manhattan, NYU Langone is composed of five hospitals—Tisch Hospital, its flagship acute care facility; Rusk Rehabilitation; the Hospital for Joint Diseases, the Medical Center’s dedicated inpatient orthopaedic hospital; NYU Lutheran Medical Center, a full-service, 450-bed teaching hospital located in Brooklyn, and Hassenfeld Children’s Hospital, a comprehensive pediatric hospital supporting a full array of children’s health services across the Medical Center. Also part of NYU Langone is NYU School of Medicine, which since 1841 has trained thousands of physicians and scientists who have helped to shape the course of medical history, and the Laura and Isaac Perlmutter Cancer Center, a National Cancer Institute–designated cancer center. The Medical Center’s trifold mission to serve, teach, and discover is achieved 365 days a year through the seamless integration of a culture devoted to excellence in patient care, education, and research. For more information, go to www.NYULangone.org
About the NYU Rory Meyers College of NursingNYU Rory Meyers College of Nursing is a global leader in nursing education, research, and practice. It offers a Bachelor of Science with a major in Nursing, a Master of Science and Post-Master’s Certificate Programs, a Doctor of Nursing Practice degree and a Doctor of Philosophy in nursing research and theory development.
About CDUHRThe mission of the Center for Drug Use and HIV Research (CDUHR) is to end the HIV and HCV epidemics in drug using populations and their communities by conducting transdisciplinary research and disseminating its findings to inform programmatic, policy, and grass roots initiatives at the local, state, national and global levels. CDUHR is a Core Center of Excellence funded by the National Institute on Drug Abuse (Grant #P30 DA011041). It is the first center for the socio-behavioral study of substance use and HIV in the United States and is located at the New York University College of Nursing. For more information, visit www.cduhr.org.
SEE ORIGINAL STUDY
Newswise —
Many women put too much pressure on themselves to make the holidays perfect for everyone. This can add a lot of unnecessary stress and anxiety that can lead to serious heart problems.
Houston Methodist DeBakey Heart & Vascular Center cardiologist Karla Kurrelmeyer, M.D. says in their quest to get everything done on time, some women will ignore the mild symptoms of a silent heart attack.“Most of the time people who are experiencing a heart attack will have pain in the chest, shortness of breath, etc. Silent heart attack symptoms might be as simple as indigestion, flu-like symptoms, or feeling discomfort like a pulled muscle in the chest or back,” Kurrelmeyer said. “It’s important to have these symptoms checked as soon as possible to avoid scarring or damage to the heart.”Kurrelmeyer says stress-induced cardiomyopathy is also a concern for women around the holidays. This occurs when women are under great amounts of stress for a short period of time and that stress is compounded with another traumatic event such as a death in the family, a car accident, loss of money, etc. If it is ignored it can be fatal.
“Stress-induced cardiomyopathy is a weakening of the left ventricle, the heart’s main pumping chamber,” Kurrelmeyer said. “It is brought on by the release of stress hormones that shock the heart, causing changes in the heart muscles that then cause the left ventricle to not work properly. The vast majority of people who are affected by this condition are women in the late 50s to mid-70s.”
Someone experiencing this condition might develop chest pains or shortness of breath after severe stress, either emotional or physical, she said. In most cases, it is treated with medication such as beta blockers or ACE inhibitors. It’s important to have an echocardiogram as soon as possible if you are experiencing any symptoms.
A spike in blood pressure is also commonduring the holidays. Kurrelmeyer says many women end up in the ER with chest pains or palpitations and, in the most severe cases, can suffer a stroke. If a woman has a history of high blood pressure it’s important to monitor it closely, especially during those times when the stress level rises.
Heart problems in women are not usually as recognizable as they are in men. Some of the symptoms for women include:• Extreme weakness, anxiety, or shortness of breath.• Discomfort, pressure, heaviness or pain in the chest, arm, below the breastbone or in the middle of the back.• Sweating, nausea, vomiting, dizziness.• Fullness, indigestion, a tightness in the throat area.• Rapid or irregular heartbeats.
“It’s important to take time for yourself during the holiday season and do things that will help relieve your stress,” Kurrelmeyer said. “Exercise, either walking or running, yoga, meditation, a nice walk with a loved one, whatever it takes, make it happen. The holidays should be a joyous time spent with family and friends at home, not with doctors in an emergency room.”
Newswise — DALLAS –
The nation’s largest statewide effort to track concussions among youth athletes is under way in Texas with the launch of a registry designed to assess the prevalence of brain injuries in high school sports.
The ConTex registry – a partnership between the University Interscholastic League(UIL) and the UT Southwestern Peter O’Donnell Jr. Brain Institute – will fill a major gap in concussion research and is expected to provide a gauge for whether certain rules or equipment changes are improving player safety.
The registry may also provide a blueprint for other states considering similar efforts and could be a key step in creating a nationwide database for concussions. Such a project was recently proposed by the U.S. Centers for Disease Control and Prevention.
“This is a groundbreaking initial step. I think we’re on the verge of a very impactful project that will inform the nation about the frequency of concussions and will provide basic information about concussion and recovery in student-athletes,” said Dr. Munro Cullum, Professor of Psychiatry, Neurology and Neurotherapeutics and Neurological Surgery with the O’Donnell Brain Institute at UT Southwestern Medical Center.
The UIL, which regulates athletics in Texas public schools, has partnered with the O’Donnell Brain Institute to implement the registry, which will complement studies in other age groups. While the NCAA, NHL, NFL and other professional sports organizations are tracking the issue in the college and professional ranks, little has been done on a scale as large as Texas to evaluate concussions in youth athletics.
The registry in Texas – which leads the U.S. with more than 800,000 students participating in high school sports – will include player concussion cases reported by middle and high school athletic trainers in all UIL-sanctioned athletic activities.
“The health and safety of our student participants is at the forefront of everything we do,” said Charles Breithaupt, UIL Executive Director. “The UIL Medical Advisory Committee has been focused on concussions since its inception 15 years ago and this concussion registry will provide valuable information and help us continue to improve the safety of extracurricular athletics.”
The ConTex project is modeled after a smaller concussion study (ConTex1) that Dr. Cullum helped launch last year that tracks more detailed information about concussions in the Dallas-Fort Worth area. He also led a first-of-its-kind studypublished last year that found NFL players who lost consciousness due to concussion showed key differences in brain structure later in life.
The statewide registry relies on athletic trainers and school personnel across Texas to report all concussions that occur in UIL athletics to a central database through an app or online site developed by Medical Innovation Labs in Austin. Among the information being tracked is the cause of the injury, concussion history, the gender of the player and other data. During this school year, UIL-member schools will participate on a voluntary basis, with plans to expand reporting next school year.
Dr. Cullum, the principal investigator of both ConTex studies, said his team will measure how often concussions occur in each sport, identify areas with low rates, and with more data eventually examine whether certain practices are helping reduce concussions or shorten recovery times in those areas.
Children under age 15 account for the most traumatic brain injury visits to the emergency room, according to CDC findings released in July from a national survey of hospital records. Because there is no system in place to fully assess the prevalence of concussions in youth athletics, the CDC is seeking federal funding to establish a national database.
“A lot of states will follow suit if they’re not already working on this very topic,” said Dr. Cullum, a neuropsychologist who holds the Pam Blumenthal Distinguished Professorship in Clinical Psychology. “I do think our registry will develop a very strong groundwork for a national registry.”
All 50 states have passed legislation in recent years to address concussions in extracurricular athletics, but few have successfully launched statewide registries to track such injuries in all sports. Hawaii, for instance, launched its own registry in 2010, but the data have been relatively limited, with only 67 high schools participating. Colorado, Arizona and Maine have more recently launched their own. The UIL will be the first association of its kind to launch a registry of this magnitude.
Researchers expect the broader statistics gathered in Texas will give substantial insight into the prevalence of concussions in student-athletes and quickly benefit other clinical and research efforts at the O’Donnell Brain Institute. This benefit will include an array of neurological studies involving current and former NFL players, education outreach in schools, and a new sports concussion return-to-play clinic that promotes medically monitored exercise during recovery.
The statewide registry is funded through UT Southwestern’s Texas Institute for Brain Injury and Repair, which was established with $7.5 million in annual funding from the Texas Legislature to explore the full spectrum of brain injuries from strokes to spinal cord injuries.
Questions about the registry can be emailed to ConTex@UTSW.edu.
Concussion Extras
QA: Impact of Texas registry
Blog: Athletes who sandbag on concussion tests
Video: UTSW, Cowboys on concussion outreach
Contact: Email
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty includes many distinguished members, including six who have been awarded Nobel Prizes since 1985. The faculty of almost 2,800 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide medical care in about 80 specialties to more than 100,000 hospitalized patients and oversee approximately 2.2 million outpatient visits a year.
Newswise —
Inflammation is a good thing when it’s fighting off infection, but too much can lead to autoimmune diseases or cancer. In efforts to dampen inflammation, scientists have long been interested in CC chemokine receptor 2 (CCR2) — a protein that sits on the surface of immune cells like an antenna, sensing and transmitting inflammatory signals that spur cell movement toward sites of inflammation. Researchers at the Skaggs School of Pharmacy and Pharmaceutical Sciences at University of California San Diego have now determined the 3D structure of CCR2 simultaneously bound to two inhibitors. Understanding how these molecules fit together may better enable pharmaceutical companies to develop anti-inflammatory drugs that bind and inhibit CCR2 in a similar manner.
The study is published December 7 by Nature.
CCR2 and associated signaling molecules are known to play roles in a number of inflammatory and neurodegenerative diseases, including multiple sclerosis, asthma, diabetic nephropathy and cancer. Many drug companies have attempted to develop drugs that target CCR2, but none have yet made it to market.
“So far drugs that target CCR2 have consistently failed in clinical trials,” said Tracy Handel, PhD, professor in the Skaggs School of Pharmacy. “One of the biggest challenges is that, to work therapeutically, CCR2 needs to be turned ‘off’ and stay off completely, all of the time. We can’t afford ups and downs in its activity. To be effective, any small molecule drug that inhibits CCR2 would have to bind the receptor tightly and stay there. And that’s difficult to do.”
Handel led the study with Irina Kufareva, PhD, project scientist at Skaggs School of Pharmacy, and Laura Heitman, PhD, of Leiden University. The study’s first author is Yi Zheng, PhD, postdoctoral researcher also at Skaggs School of Pharmacy.
CCR2 spans the membrane of immune cells. Part of the receptor sticks outside the cell and part sticks inside. Inflammatory molecules called chemokines bind the external part of CCR2 and the receptor carries that signal to the inside of the cell. Inside the cell, CCR2 changes shape and binds other communication molecules, such as G proteins, triggering a cascade of activity. As a result, the immune cells move, following chemokine trails that lead them to places in the body where help is needed.
In this study, the researchers used a technique known as X-ray crystallography to determine the 3D structure of CCR2 with two molecules bound to it simultaneously — one at each end.
That’s a huge accomplishment because, Kufareva said, “Receptors that cross the cell membrane are notoriously hard to crystalize. To promote crystallization, we needed to alter the amino acid sequence of CCR2 to make the receptor molecules assemble in an orderly fashion. Otherwise, when taken out of the cell membrane, they tend to randomly clump together. ”
Handel, Kufareva and team also discovered that the two small molecules binding CCR2 turn the receptor “off” by different but mutually reinforcing mechanisms. One of the small molecules binds the outside face of the receptor and blocks binding of the natural chemokines that normally turn the receptor "on.” The other small molecule binds the face of the receptor inside the cell, where the G protein normally binds, preventing inflammatory signal transmission. According to Handel, the latter binding site has never been seen before.
“It’s our hope that this new structure of CCR2 with two bound inhibitors will help optimize current and future drug discovery efforts,” Kufareva said.
Co-authors of this study also include: Ling Qin, Martin Gustavsson, Chunxia Zhao, Ruben Abagyan, UC San Diego; Natalia V. Ortiz Zacarías, Henk de Vries, Adriaan P. IJzerman, Leiden University; Gye Won Han, Vadim Cherezov, Raymond C. Stevens, University of Southern California; Marta Dabros, Robert Cherney, Percy Carter, Andrew Tebben, Briston-Myers Squibb Company; Dean Stamos, Vertex Pharmaceuticals.
This research was funded, in part, by the National Institutes of Health (R01GM071872, R01AI118985, R01GM117424, U54GM094618, U01GM094612, R21AI121918, R21AI122211, ACB-12002, AGM-12006).
###
SEE ORIGINAL STUDY