News
Newswise — WASHINGTON, DC─
African Americans with sleep apnea and insomnia are rarely diagnosed with either problem, even when the severity of the two sleep disorders are likely to affect their health, according to new research presented at the ATS 2017 International Conference.
“African Americans experience a disproportionate burden of numerous health problems, including obesity, diabetes, hypertension and cardiovascular disease, all of which have been shown to be associated with sleep,” said lead study author Dayna A. Johnson, PhD, MPH, MS, MSW, a postdoctoral research fellow at Brigham and Women’s Hospital and Harvard Medical School. “It seems plausible that sleep apnea and insomnia are important risk factors contributing to these health disparities.”
Dr. Johnson and her colleagues studied data of 825 African Americans who underwent a sleep study as part of the Jackson (Miss.) Heart Study, which is funded by the National Institutes of Health and is the largest single-site prospective investigation of cardiovascular disease in African Americans undertaken. The average age of those undergoing the home sleep study was 63 years, and two-thirds of the participants were women.
The researchers defined sleep apnea, which produces pauses in breathing, based on the apnea-hypopnea index (AHI), which measures the number of pauses that occur per hour of sleep. An AHI >5 was considered mild; an AHI >15, moderate; and an AHI >30, severe. The researchers used the Women’s Health Initiative (WHI) Insomnia Rating Scale, a commonly used assessment of perceived insomnia symptoms, to define insomnia. Participants with a score >10 were considered to have insomnia. Participants were asked if a physician had told them that they suffered from either of the disorders.
The study found that three of every four participants had sleep apnea: 38.4 percent had mild sleep apnea; 21.3 percent had moderate sleep apnea; and 15.8 percent had severe sleep apnea. But only 2.1 percent of those with sleep apnea reported that a physician diagnosed the condition.
Higher body mass index, hypertension, diabetes, being male and being older were all associated with sleep apnea and its severity.
The study also found that more than 2 in 10 participants suffered from insomnia. But only 6.7 percent of them reported a physician diagnosis.
According to Dr. Johnson, the prevalence of both sleep apnea and insomnia in the study population was higher than would be expected in the general population of adults of a similar age.
“There is a disturbingly high prevalence of undiagnosed sleep disorders in our study population of African Americans,” she said. “It is important to investigate the reasons for this high prevalence as well as investigate interventions targeted at increasing awareness and screening for sleep disorders.”
Because treating these sleep disorders “could drastically improve quality of life and reduce the burden of subsequent adverse health outcomes,” Dr. Johnson added, clinicians need to identify patients at risk of these sleep disorders and encourage them to undergo sleep studies. In addition, although public awareness of sleep apnea is growing, efforts targeting the most at-risk populations may be warranted.
Dr. Johnson said that study findings from the Jackson, Miss., metropolitan area may not apply to African Americans living elsewhere. “African Americans living in Jackson, Mississippi, may not be representative of all African Americans due to differences in risk factors that may be related to geography,” she said.
Contact for Media: Dayna A. Johnson, PhD, MPH, MS, MSW, djohnson@research.bwh.harvard.edu
###
Newswise —
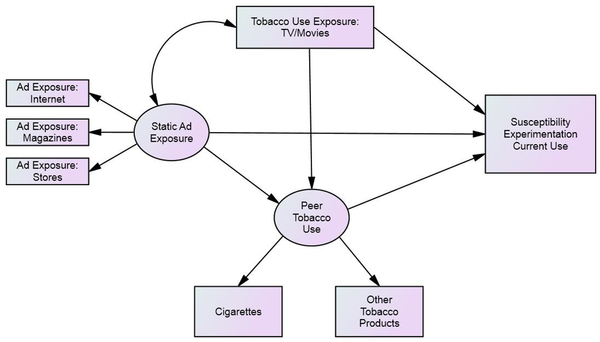
Among 12- to 17-year-olds who have never used tobacco products, nearly half were considered receptive to tobacco marketing if they were able to recall or liked at least one advertisement, report a coalition of behavioral scientists in a new national study. Receptivity to tobacco ads is associated with an increased susceptibility to smoking cigarettes in the future.Led by researchers at University of California San Diego Moores Cancer Center and Dartmouth’s Norris Cotton Cancer Center, the researchers analyzed data from the Population Assessment of Tobacco and Health (PATH) Study, which included interviews with 10,751 adolescents who reported having never used any type of tobacco product. Risk to use a tobacco product in the future was the researchers’ main point of interest. The findings are published in the May 22 issue of Pediatrics."Tobacco marketing restrictions differ by product with only e-cigarettes allowed to be advertised on television,” said John P. Pierce, PhD, Professor Emeritus in the Department of Family Medicine and Public Health at UC San Diego School of Medicine and Moores Cancer Center and lead author on the study. "Previous studies have linked receptivity to cigarette advertising with susceptibility to smoke cigarettes among youth. What we’re seeing in this study is that even being receptive to marketing of non-cigarette tobacco products, including e-cigarettes, is associated with susceptibility to smoke cigarettes.”In this analysis of the first wave of data from the PATH Study, respondents were considered susceptible to tobacco or committed to never using these products based on responses to three questions assessing their curiosity about the product, intention to try it in the near future, and likely response if a best friend were to offer them the product. Only those with the strongest rejection to all three questions were categorized as committed to never use. All others were susceptible. This index has been validated in multiple studies.Participants were shown 20 tobacco ads chosen randomly from 959 ads representing all available recent commercials used in print, direct mail, internet or television advertisements. Each respondent was asked initially to name his or her favorite tobacco ad and then shown a random set of five ads for each of the following products: cigarettes, e-cigarettes, cigars and smokeless products. For each ad presented, they were asked if they had seen the ad in the past 12 months and whether they liked the ad. Aided recall was classified as low receptivity while image-liking or favorite ad was considered to be higher.A high proportion of under-aged adolescents in the United States are still exposed to tobacco advertising. The study found that 41 percent of 12- to 13-year-olds, and about half of both 14- to 15-year-olds and 16- to 17-year-olds were receptive to any type of tobacco advertising. "Six of the top 10 most recognized tobacco ads by adolescents were for e-cigarettes, four of which were aired on TV," said James Sargent, MD, director of the C. Everett Koop Institute at Dartmouth and co-author. "The PATH Study will continue to track these adolescents who have not used tobacco and will be able to identify if receptivity to marketing for different tobacco products during wave 1 of the study — particularly e-cigarette marketing — increases cigarette smoking one or two years later."Receptivity to advertising was highest for e-cigarettes with 28 to 33 percent across age groups, followed by 22 to 25 percent for cigarettes and 15 to 21 percent for cigars. E-cigarette advertising is of interest to researchers because of its presence on television and because showing people vaping is very similar to showing people smoking, said Pierce. The proportion who were susceptible to using tobacco products increased with the level of receptivity. Fifty percent of respondents considered to have low receptivity, 65 percent who were moderately receptive and 87 percent of youth who were deemed highly receptive were susceptible to use tobacco products.“Cigarette smoking is still a major problem and a major cause of lung cancer and other diseases,” said Pierce. “We’ve had big declines in the number of people who initiated smoking, but it is important that we maintain that reduction.”Co-authors include: Martha White, David R. Strong, Eric Leas, Madison Noble, Dennis Trinidad, Karen Messer, UC San Diego; Nicolette Borek, David B. Portnoy, Blair N. Coleman, US Food and Drug Administration; Victoria R. Green, National Institutes of Health and Kelly Government Solutions; Annette R. Kaufman, National Cancer Institute; Cassandra A. Stanton, Westat and Georgetown University Medical Center; Maansi Bansal-Travers, Andrew Hyland, Roswell Park Cancer Institute; Jennifer Pearson, Johns Hopkins University and Schroeder Institute for Tobacco Research and Policy Studies at Truth Initiative; Meghan B. Moran, Johns Hopkins University; and Charles Carusi, Westat. This research was funded by the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services, under a contract to Westat, which collected data using Audio-Computer-Assisted Self Interviews.
###
Newswise — LOS ANGELES –
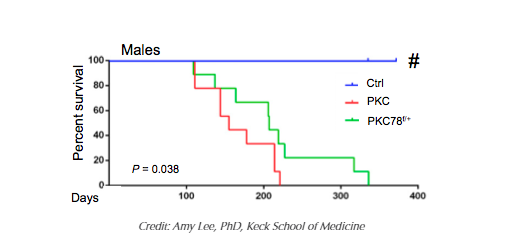
New research from the Keck School of Medicine of the University of Southern California (USC) shows new promise in the fight against one of the most lethal forms of cancer. Studies in mice with a mutation present in 90 percent of pancreatic cancer patients (the KRAS mutation) indicate that expressing only half the amount of the glucose-regulated protein GRP78 is enough to halt the earliest stage of pancreatic cancer development.
The study, funded in part by the National Institutes of Health, suggests that because the protein is required for “switching” healthy pancreatic cells that produce enzymes to digest food into potentially cancerous cells, reducing the amount of this protein delays pancreatic cancer development and prolongs survival. The study, published online on May 16 in the Proceedings of the National Academy of Sciences of the United States of America, is the first to establish the pivotal role of the protein in pancreatic cancer.
“Cancer cells are addicted to high levels of GRP78 for cancer development and growth. Our hope is that partially reducing or inactivating the protein by therapeutic agents could one day be an effective complementary therapy for pancreatic cancer and other cancers, while sparing other healthy organs,” said Amy Lee, PhD, professor of biochemistry and molecular medicine at the Keck School and the Judy and Larry Freeman Chair in Basic Science Research at the USC Norris Comprehensive Cancer Center.
Lee, who was the first scientist to clone human GRP78, has since dedicated much of her research to investigating the protein’s role in cancer progression and treatment. For her scientific contributions, Lee was honored by a MERIT award from the National Cancer Institute and elected as Fellow of the American Association for the Advancement of Science.
“As developing drugs directly targeting the KRAS genetic mutation has been challenging, we are thrilled these findings indicate that we can attack KRAS-driven pancreatic cancer through an entirely new method,” Lee said.
GRP78 is a stress-inducible protein that folds newly synthesized proteins and performs quality control in the endoplasmic reticulum (an essential component of human cells). During stress, a fraction of GRP78 is shipped out to the cell surface to perform additional growth and survival functions. Cancer cells, particularly those that survive treatment, typically undergo more stress than healthy cells, resulting in increased levels of GRP78 to help the cancer cells survive, grow and develop therapeutic resistance.
A number of studies across cancer types have shown a relationship between highly elevated levels of the protein and increased risk for cancer recurrence or decreased survival. With GRP78 emerging as an attractive anti-cancer target, there is active development of potential treatments that can inhibit GRP78 activity or expression, including some that are in early-phase clinical trials with promising results. Certain food and herbs, including green tea and soy, contain natural compounds that can suppress the protein, Lee said.
Patients and physicians alike are eager for more effective treatments for pancreatic cancer, as it is among the deadliest forms of cancer. According to the American Cancer Society, more than 53,600 people will be diagnosed with pancreatic cancer this year, and more than 43,000 people will die from the disease. The five-year survival rate for early stage pancreatic cancer is only 12 percent, compared to 100 percent for breast cancer and prostate cancer and 92 percent for colon cancer.
“Translating any basic science discovery into clinical practice is a long process that requires substantial resources,” Lee said. “But given the notorious difficulties of treating KRAS-mutation related cancers, particularly in a disease as devastating as pancreatic cancer, this research provides hope and a novel approach. I am excited to put our theories to test in the clinical setting.”
###
Newswise — The Valley Heart and Vascular Institute in Ridgewood, NJ, has been selected as 1 of just 10 hospitals – and the only hospital in New Jersey – to participate in a nationwide study investigating a minimally invasive aortic valve replacement procedure for individuals with aortic stenosis.
The first-of-its-kind clinical trial, led by Medstar Washington Hospital Center in Washington, D.C., aims to evaluate the use of transcatheter aortic valve replacement (TAVR), a minimally invasive procedure, in aortic stenosis patients who are at low risk for conventional open-heart surgery. TAVR is not yet approved by the FDA for use in this population. TAVR has already been established as a treatment option for intermediate- and high-risk patients. The trial is now open and will be enrolling 200 patients over a 24-month period. It will be non-randomized, meaning individuals who qualify will be selected to undergo the TAVR procedure instead of open-heart surgery.
"TAVR has already been shown to extend lives and improve the quality of life for intermediate- and high-risk patients who just a few years ago may not have had an alternative to open-heart surgery,” said John Goncalves, M.D., Director of Cardiac Surgery at The Valley Hospital and Surgical Director of Valley’s TAVR Program. “This is an exciting study to be a part of because it may potentially prove the effectiveness of TAVR for low-risk patients and open the door for others to qualify for this minimally invasive procedure in the future.”
TAVR is a procedure used to treat aortic stenosis, a life-threatening condition that occurs when blood flow is obstructed due to the narrowing of the aortic valve, one of the valves in the heart. Using TAVR, the heart team can replace a diseased aortic heart valve in a less-invasive manner than with open-heart surgery. The procedure requires only a small incision in the groin, through which an expandable heart valve is placed into the body and up to the heart via a catheter-based delivery system. Studies have shown that patients achieve better outcomes when undergoing TAVR than with medication alone.
“We are honored to be recognized for our expertise and experience with the TAVR procedure,” said Dr. Goncalves. “Clinical trials like this are critical to our work providing the highest quality and most innovative care for our patients.”
Individuals interested in making an appointment for an evaluation to see if they are a candidate for this study are encouraged to contact Jaclyn Chomsky, D.N.P., Valve Coordinator at Valley, at 201-447-8378 or chomja@valleyhealth.com.
Newswise —
Social media is more than a way to connect with friends, access news or information, or watch entertaining videos. It’s now a proven method of conducting medical research.
Researchers in the Urology department at Beaumont Hospital, Royal Oak, Michigan collaborated with the Interstitial Cystitis Association to use social media to recruit research volunteers for a study leading to the development of a new urine biomarker for the diagnosis of interstitial cystitis. IC causes recurring pelvic pain, pressure or discomfort in the bladder and pelvic region, often associated with urinary frequency and urgency. In extreme cases, patients with IC may urinate 60 times a day or more.
The social media research exceeded expectations. Within just two weeks, 454 women and men from 46 states participated in the study, watching a YouTube video and completing an online survey. Qualified participants were sent a prepaid return shipping container to provide a urine sample. The container included preservatives to maintain protein and nucleic acid in the urine at room temperature.
Analysis of the samples led to the discovery of three proteins that were highly statistically different for research participants with IC with ulcer versus those without ulcer. This was then used in a machine-learning program to accurately classify patients with the disease.
The research was presented May 13 at the American Urological Association meeting in Boston, the largest meeting of urologic specialists in the world.
IC is a disease that affects more than 12 million people in the U.S. and currently does not have a single, objective laboratory test for diagnosis.
Laura Lamb, Ph.D., urology research scientist at Beaumont, said “Our goal was to develop a simple urine-based test that identifies IC patients with bladder pain syndrome who have ulcerative IC and a bladder permeability defect. The test had to be developed and validated in a large number of samples collected beyond the referral area of our single academic medical center.”
Participants were recruited through a collaboration with the Interstitial Cystitis Association, which has an active presence across several social media platforms.
“IC is ideal for social media research,” said Kenneth Peters, M.D., chief of Urology, Beaumont, Royal Oak. “The IC community is a motivated patient group because of their poor quality of life. They are relatively younger compared to patients with other chronic diseases; as such, they may be more comfortable and familiar with the internet and social media.”
The use of social media is an emerging approach for medical researchers to rapidly collect, process and interpret data, generating support for medical advances that would otherwise be impossible due to research funding constraints and the large number of participants needed for medical research.
Michael Chancellor, M.D., director of Neurourology at Beaumont, Royal Oak, predicts that, “As the research community discovers this new role of social media, medical research may no longer be confined to academic centers, but will be a collaboration of key stakeholders across the world.”
“Our study achieved diversity in sample source collection from across the U.S. and engaged many national stakeholders using social media,” said Dr. Chancellor. “And the outcome of the study is significant - the development of a bladder permeability risk score that is the first validated urine biomarker test for interstitial cystitis/bladder pain syndrome.”
The research was supported with funding from the Taubman Family through the Taubman Interstitial Cystitis Research Program.
# # #
Newswise — Washington, DC –
Pasta is a convenient, nutritious, easy-to-prepare meal for families. Pasta pleases even the pickiest of young eaters. And now, even more good news: new research shows that pasta consumption in children and adolescents is associated with a better diet quality than that of children who do not eat pasta. The research, which was presented at the 2017 Experimental Biology conference at the end of April in Chicago, demonstrated that young pasta-eaters have greater intakes of important vitamins and minerals and lower intakes of saturated fat and total fat in the diet compared to their peers who do not consume pasta.
The research, “Pasta Consumption in American Children and Adolescents is Associated with Greater Daily Intake of Shortfall Nutrients as Defined by the 2015 Dietary Guidelines, Improved Diet Quality and Lower Added Sugar Intake,” was conducted by Nutritional Strategies, Inc. on behalf of the National Pasta Association. The study examined associations between pasta consumption, shortfall nutrient intakes as defined by the 2015 Dietary Guidelines (2015 DG) and diet quality in comparison to non-pasta consumption in U.S. children and adolescents (ages 2-18). Pasta consumption was defined as all dry domestic and imported pasta/noodle varieties made with only wheat and no egg. The data review did not look at any health outcomes associated with pasta consumption except for the ones specified below.
From the analysis, researchers identified a number of key positive nutritional dietary patterns associated with children and adolescents who eat pasta as part of their diet compared to those who don’t eat pasta. They are:
Better overall diet quality (as measured by USDA’s Healthy Eating Index-2010 scale)
Greater intake of key shortfall nutrients like dietary fiber, folate, iron, magnesium and vitamin E
Lower daily intakes of saturated fat and total fat
No significant associations were seen with body weight, waist circumference and body mass index
Pasta has long been celebrated as one of America’s favorite foods and is advocated by nutritionists for its good nutrition.
“Good nutrition is critical to the developing minds and bodies of children and adolescents. Certain grain foods, like pasta, are a great complement to a healthy well-balanced meal and provide plenty of opportunities for improving the diet,” explains registered dietitian Diane Welland, Nutrition Communications Manager for the National Pasta Association. “Think of pasta as a canvas from which you can add nutrient-dense, fiber-rich foods like fresh vegetables, fruits, cheese, lean meats and legumes, when creating meals for your family.”
For more information, recipes and facts about pasta, please visit www.pastafits.org. To learn more about the research, please contact Kara Yacovone at kyacovone@kellencompany.com.
About the National Pasta Association (NPA):
NPA is the leading trade association for the U.S. pasta industry. The association provides leadership to the industry on public policy issues, serving as its voice in Washington, D.C. NPA also forges alliances with key organizations, monitors and addresses technical issues and conducts nutrition and food safety research on behalf of the U.S. pasta industry.
www.pastafits.org
# # #
Newswise —
Combining risk scores helps clinicians better identify atrial fibrillation patients who face increased risks of developing dementia, researchers have found.
Combining the Intermountain Mortality Risk Score (IMRS), developed by clinicians at Intermountain Healthcare, with the traditional CHA2DS2-VASc risk score, was more accurate in identifying at-risk patients than using the traditional score alone, according to new research from the Intermountain Medical Center Heart Institute in Salt Lake City.
Previous studies have linked atrial fibrillation patients who have a high CHA2DS2-VASc score with increased risk of stroke and dementia, but this new research examined patients with low CHA2DS2-VASc scores to better identify those at higher risk of dementia.
The CHA2DS2-VASc score is an international guideline to determine a patient’s need for blood thinner. Points are added based on age, sex, and history of stroke, hypertension, heart failure, or diabetes. An atrial fibrillation patient with a score of two or more is placed on blood thinners.
“Patients who have a CHA2DS2-VASc score of zero or one are considered at low risk for developing dementia when using the traditional CHA2DS2-VASc tool,” said Kevin Graves, lead author of the study and researcher with the Intermountain Medical Center Heart Institute. “But when the IMRS tool is used to evaluate those same patients, a better picture is provided to physicians that shows which patients are truly at a high risk for dementia.”
The Intermountain Mortality Risk Score is based on lab values that are typically collected from a patient – a complete blood count (CBC) and basic metabolic profile (BMP) – which sync automatically to a patient’s electronic medical record so physicians have the score readily available to them.
Results of the study will be presented during the Heart Rhythm Society’s annual conference in Chicago on Thursday, May 11.
Nearly 75,000 atrial fibrillation patients who had no history of dementia were included in the retrospective study. After they received an atrial fibrillation diagnosis, patients were grouped together according to their CHA2DS2-VASc score of one, two, or three or greater. Patients were then further organized in their groupings using the IMRS.
Atrial fibrillation is the most common abnormal heart rhythm that affects more than 2.7 million Americans.
“We don’t consider atrial fibrillation to be a risk factor for dementia, but rather a risk marker,” said Graves. “Dementia may be an endgame of the underlying atrial fibrillation diagnosis, so as that disease progresses, the risk of dementia goes up significantly. Having the best tools available to identify risks can help physician and patients be better equipped in the shared decision-making process to help them prevent, postpone, or better manage the symptoms of dementia.”
Members of the Intermountain Medical Center Heart Institute team involved in the study include Benjamin Horne, PhD; Heidi May, PhD; Tami Bair, RN; Victoria Jacobs, PhD; Brian Crandall, MD; Michael Cutler, DO, PhD; Charles Mallender, MD; Jeffrey Osborn, MD; Peter Weiss, MD; John D. Day, MD; and Jared Bunch, MD.
Intermountain Medical Center Heart Institute is part of the Intermountain Healthcare system, which is based in Salt Lake City.
###
Newswise —
Hepatitis C infections among pregnant women nearly doubled from 2009-2014, likely a consequence of the country’s increasing opioid epidemic that is disproportionately affecting rural areas of states including Tennessee and West Virginia.
Injection drug use is the main risk factor for the hepatitis C virus, now the country’s most common blood-borne infection with an estimated 3.5 million people living with chronic infection.
“We have seen a dramatic increase in opioid use in pregnancy and in the number of infants having drug withdrawal,” said lead author Stephen Patrick, M.D., assistant professor of Pediatrics and Health Policy at Vanderbilt University Medical Center.
“Taken together, this suggests that efforts targeted at preventing and expanding treatment for opioid use disorder may help mitigate some of the increases we see,” Patrick said.
Patrick co-authored a study with the Tennessee Department of Health (TDH) that was released today in the Center for Disease Control and Prevention’s weekly epidemiological digest Morbidity and Mortality Weekly Report (MMWR).
Hepatitis C infection present at the time of delivery increased 89 percent, from 1.8 to 3.4 per 1,000 live births from 2009-2014, equaling 35 infants a day exposed to the virus.
Authors reported notable increases in rural counties in Tennessee and in rural states like West Virginia, which had the highest infection rate in 2014 (22.6 per 1,000 live births).
“We found substantial state-to-state variation in hepatitis C infection rates,” Patrick said. “West Virginia had the highest prevalence of infection among pregnant women — 1 in 50 newborns were exposed to the virus.”
In Tennessee, the odds of a hepatitis C infection at birth were approximately threefold higher for women residing in rural counties, 4.5-fold higher for women who smoked cigarettes during pregnancy, and nearly seventeenfold higher for women with concurrent hepatitis B virus infection.
Tennessee had 10.1 hepatitis C infections per 1,000 live births in 2014.
“We found that rural and Appalachian counties were particularly impacted by the virus,” Patrick said. “In some counties in Tennessee, nearly 8 percent of pregnant women were documented as being infected with hepatitis C at the time of delivery.”
Senior author and TDH Medical Director for HIV, STD & Viral Hepatitis Carolyn Wester, M.D, said the increase highlights the importance of ensuring that women of childbearing age have access to hepatitis C testing and treatment.
Patrick agreed, noting that women who know they have the virus before pregnancy can be treated to hopefully clear the virus prior to becoming pregnant.
He also said that it is increasingly important that infants exposed to hepatitis C are monitored to see if they get the virus.
“We need to build systems of care to ensure that all infants exposed to the virus are adequately followed,” Patrick said.
TDH State Epidemiologist Tim Jones, M.D., said the study is an important reminder of the threat of this growing epidemic to high-risk populations throughout the U.S.
“While this study focuses on pregnant women and a high-risk area in Tennessee, it is also important to remember that hundreds of thousands of people throughout the U.S. have hepatitis C, and a large percentage of them do not know it,” Jones said.
“Anyone born between 1945-1965, or who has ever used IV drugs, or is otherwise worried about hepatitis infection, is encouraged to discuss with their clinicians whether testing may be appropriate for them,” he said.
Newswise —
Researchers at the Johns Hopkins Bloomberg School of Public Health’s Center for a Livable Future calculated the nutritional value of food wasted in the U.S. at the retail and consumer levels, shining a light on just how much protein, fiber and other important nutrients end up in the landfill in a single year.
These lost nutrients are important for healthy diets, and some — including, dietary fiber, calcium, potassium and vitamin D — are currently consumed below recommended levels. Nutrient-dense foods like fruits, vegetables, seafood and dairy products are wasted at disproportionately high rates.
Previous research estimated that as much as 40 percent of food is wasted nationally, but it wasn’t clear before this study how nutritious that food was. While not all wasted food is consumable, a sizeable amount is, leaving researchers and policymakers looking for ways to minimize the amount of good food that gets tossed as millions of Americans go hungry, do not get enough nutrients or do not have access to healthy food options. The U.S. Department of Agriculture (USDA) and Environmental Protection Agency have set a goal of reducing food waste by 50 percent by 2030.
The findings will appear online May 15 in the Journal of the Academy of Nutrition and Dietetics.
“Huge quantities of nutritious foods end up in landfills instead of meeting Americans’ dietary needs,” says study lead author Marie Spiker, MSPH, RD, a CLF-Lerner Fellow at the Johns Hopkins Center for a Livable Future and a doctoral candidate in the Bloomberg School's Department of International Health. “Our findings illustrate how food waste exists alongside inadequate intake of many nutrients.”
For their study, the researchers calculated the nutritional value of the retail- and consumer-level food waste of 213 commodities in 2012, using data from the USDA’s Loss-Adjusted Food Availability data series. The research team, looking at 27 nutrients in all, found that food wasted in the U.S. food supply that year contained 1,217 calories, 33 grams of protein, 5.9 grams of dietary fiber, 1.7 micrograms of vitamin D, 286 milligrams calcium and 880 milligrams potassium per person, per day.
Nutrient loss estimates provided by this study could contribute to a baseline for measuring future progress, the authors say.
The study also highlights how the amount of nutrients lost to waste compares to nutritional deficits in the typical American diet. For example, dietary fiber is important for maintaining digestive health and is found in grains, vegetables and fruits. Researchers estimate that, in 2012, food wasted each day contained upwards of 1.8 billion grams of dietary fiber, which is comparable to the full recommended intake for dietary fiber for 73.6 million adult women. American women under-consumed dietary fiber by 8.9 grams per day in 2012. The study found that the daily amount of wasted dietary fiber is equivalent to the amount needed to fill this nutritional gap for as many as 206.6 million adult women.
Many factors contribute to food waste at both the retail and consumer levels, including the disposal of food due to aesthetic standards, large portion sizes, and management of perishables in fridges and pantries. There is currently great energy around efforts to address waste of food. Preventing waste at the source is considered to be the optimal approach. Strengthening food recovery efforts that bring surplus food to food banks and pantries is also an important area of effort, innovation and impact.
“This study offers us new ways of appreciating the value of wasted food. While not all food that is wasted could or should be recovered, it reminds us that we are dumping a great deal of high quality, nutritious food that people could be enjoying,” says Roni Neff, PhD, an assistant professor in the Bloomberg School’s Department of Environmental Health and Engineering who oversaw the study and directs the CLF’s Food System Sustainability & Public Health Program. “We should keep in mind that while food recovery efforts are valuable, food recovery doesn’t get to the heart of either the food insecurity problem or the waste problem. We need strategies addressing these challenges at multiple levels.”
“Wasted Food, Wasted Nutrients: Nutrient loss from wasted food in the US and comparison to gaps in dietary intake” was written by Marie L. Spiker, Hazel A. B. Hiza, Sameer M. Siddiqi and Roni A. Neff.
This research was funded by the GRACE Communications Foundation. M. L. Spiker and S. M. Siddiqi were also supported by the CLF-Lerner Fellowship.
Newswise —
The American Cancer Society estimates that in 2017 there will be an estimated 1,688,780 new cases of cancer in the U.S. This will include about 56,870 new cases of thyroid cancer (42,470 in women, and 14,400 in men).
A number of environmental, genetic, and gender- or age-related factors may increase a person’s risk for developing thyroid cancer. While it can occur at any age, approximately two out of three cases are diagnosed in people age 20 to 55. Women are three times more likely to develop thyroid cancer than men. Seattle Cancer Care Alliance offers treatment for people who have been diagnosed with endocrine cancers, especially of the thyroid, parathyroid, and adrenal glands. Patients at Seattle Cancer Care Alliance are taken care of by doctors, advanced practice providers, and registered nurses who specialize in thyroid cancer, lead clinical trials, and provide access to the latest therapies and treatments. To arrange an interview with an SCCA physician regarding risk factors, clinical trials and treatment options or the latest U.S. Preventive Services Task Force guidelines, please contact Karen Brandvick-Baker at Seattle Cancer Care Alliance, 206.288.7239, kbrandvi@seattlecca.org.
SCCA is an NCI designated cancer center. It is ranked among the top 10 in the nation for cancer treatment of adults by U.S. News & World Report for 2016-2017.