Highlights
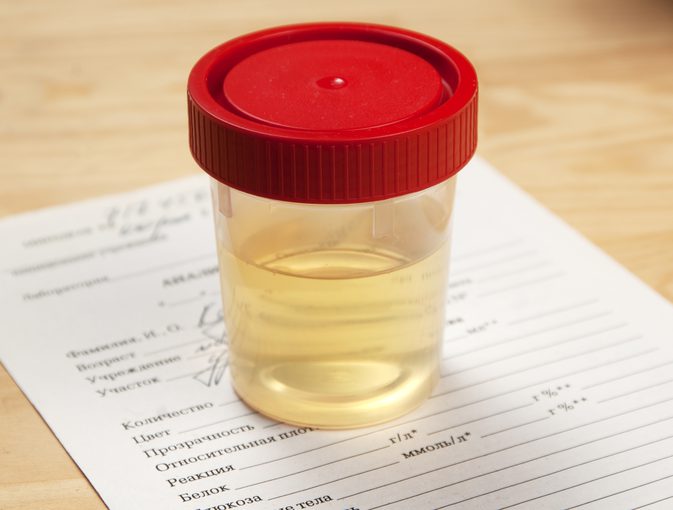
- The blood pressure–lowering medication ramipril reduced protein excretion—or proteinuria—in children with chronic kidney disease.
- Greater reductions in proteinuria during the first months of treatment were linked with a lower risk of kidney disease progression.
Newswise — Washington, DC (June 21, 2018) — In a study of children with chronic kidney disease (CKD), blood pressure medications reduced protein excretion in the urine, which was linked with a lower risk of disease progression. The findings, which appear in an upcoming issue of the Journal of the American Society of Nephrology (JASN), provide valuable information for monitoring and treating pediatric patients with CKD.
The excretion of protein in the urine, or proteinuria, indicates an increased risk for kidney and heart problems, and it is known in adult patients that this risk can be lowered with medications called angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers. Both types of drugs cause blood vessel relaxation and a decrease in blood pressure. It has not been clear, however, whether these medications benefit children with proteinuria.
To investigate, Sophie van den Belt, MD, PhD (University Medical Center Groningen, in The Netherlands) and her colleagues analyzed data from the Effect of Strict Blood Pressure Control and ACE inhibition on the Progression of CRF in Pediatric Patients (ESCAPE) trial. This trial investigated whether intensified blood pressure control can delay the progression of chronic kidney disease (CKD) in children with the condition.
In total, 280 children with CKD stage 2–4 received a fixed dose of the ACE inhibitor ramipril and were subsequently randomized to conventional or intensified blood pressure control with antihypertensive medications. The average initial proteinuria lowering was 40.2% in the conventional blood pressure control group and 46.7% in the intensified blood pressure control group. Due to the similar initial proteinuria change in the 2 study arms, the groups were combined for further analysis. The investigators found that ramipril therapy lowered proteinuria by an average of 43.5%. Also, a higher degree of proteinuria lowering during the first months of treatment was linked with a lower risk of CKD progression.
“The results indicate that a higher initial proteinuria reduction with ACE inhibition is independently associated with long-term preservation of renal function in children with CKD. This finding suggests that proteinuria lowering is an important target in the management of pediatric CKD,” said Dr. van den Belt.
Study co-authors include Hiddo Lambers Heerspink, PharmD, PhD, Valentina Gracchi, MD, PhD, Dick de Zeeuw, MD, PhD, Elke Wühl, MD, PhD, and Franz Schaefer, MD, PhD, for the ESCAPE trial group.
Disclosures: The ESCAPE study was supported by grants of the Boehringer Ingelheim Stiftung, the European Commission (5th Framework Programme QLRT-2001-00908, the Kuratorium für Dialyse und Nierentransplantation e.V., Neu-Isenburg, and the Baxter Extramural Grant Program. The study protocol was developed exclusively by the participants. Onsite monitoring of study data collection was performed by an independent clinical research organization (Omnicare Clinical Research). Aventis Pharmaceuticals supplied ramipril and financed the GCP audit. Dr. Schaefer reports serving as a paid advisor for Abbvie, Astellas, and Bayer. No other potential conflicts of interest relevant to this article were reported.
The article, entitled “Early proteinuria lowering by ACE inhibition predicts renal survival in children with chronic kidney disease,” will appear online at http://jasn.asnjournals.org/ on June 21, 2018, doi: 10.2215/ASN.2018010036.
The content of this article does not reflect the views or opinions of The American Society of Nephrology (ASN). Responsibility for the information and views expressed therein lies entirely with the author(s). ASN does not offer medical advice. All content in ASN publications is for informational purposes only, and is not intended to cover all possible uses, directions, precautions, drug interactions, or adverse effects. This content should not be used during a medical emergency or for the diagnosis or treatment of any medical condition. Please consult your doctor or other qualified health care provider if you have any questions about a medical condition, or before taking any drug, changing your diet or commencing or discontinuing any course of treatment. Do not ignore or delay obtaining professional medical advice because of information accessed through ASN. Call 911 or your doctor for all medical emergencies.
Since 1966, ASN has been leading the fight to prevent, treat, and cure kidney diseases throughout the world by educating health professionals and scientists, advancing research and innovation, communicating new knowledge, and advocating for the highest quality care for patients. ASN has more than 18,000 members representing 112 countries. For more information, please visit www.asn-online.org or contact the society at 202-640-4660.